

Abstract
The present study aimed to evaluate the use of tumescent local anesthesia or epidural anesthesia associated with an intercostal nerve block in bitches submitted to mastectomy. Fourteen bitches from the clinical routine of the Veterinary Hospital of the Federal University of Pelotas were premedicated with acepromazine (0.03 mg/kg) and morphine (0.3 mg/kg) intramuscularly, then induced with propofol (2 to 6 mg/kg/IV) and maintained with 1,4V% isoflurane (calibrated vaporizer). The patients were randomly allocated into: GALT Group (n=7), which received tumescent local anesthesia (0.16%) at the dose of 15 mL/kg, and the GEBI Group (n=7) which received epidural anesthesia with lidocaine (5 mg/kg) and morphine (0.1 mg/kg) associated with an intercostal nerve block from the 6th to 12th intercostal space with lidocaine (2 mg/kg). An increase higher than 10% in heart rate, respiratory rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure were considered as possible signs of nociception, to which fentanyl was administered intravenously as rescue analgesia. Postoperative analgesia was evaluated by means of the modified Glasgow scale at 30, 60, 120, 240 and 360 minutes. There were no differences in physiological parameters (0>0.05) in the transoperative period intra-group and inter-group the groups. The GEBI Group required more frequent transoperative rescue analgesia (9) in comparison to the GALT Group (5), but with no statistical difference. During the postoperative period, there was no need for rescue analgesia in either group. Results suggest that epidural anesthesia associated with intercostal nerve block can be used as an alternative technique in patients with restrictions against the use of local tumescent anesthesia.
Keywords: mammary tumors, pain, locoregional anesthesia, opioid.
Resumo
O presente estudo objetivou avaliar o uso da anestesia local tumescente ou da anestesia epidural associada ao bloqueio intercostal em cadelas submetidas à mastectomia. Foram utilizadas 14 cadelas, provenientes da rotina do Hospital de Clínicas Veterinária da Universidade Federal de Pelotas, pré-medicadas com acepromazina (0,03 mg/kg) e morfina (0,3 mg/kg) intramuscular, induzidas com propofol (2 a 6 mg/Kg/IV) e mantidas com isofluorano à 1,4 V% (vaporizador calibrado). Após essa etapa, foram alocadas aleatoriamente em grupo GALT (n=7), que recebeu a anestesia local tumescente 0,16% na dose de 15 mL/Kg e em grupo GEBI (n=7), que recebeu como tratamento a anestesia epidural com lidocaína (5 mg/kg) e morfina (0,1 mg/kg) associada ao bloqueio intercostal, do 6º ao 12º espaço intercostal, com lidocaína (2mg/kg). Os parâmetros avaliados para sinais de nocicepção transcirúrgica e realização de resgates analgésicos com fentanil foram: frequência cardíaca, frequência respiratória, pressão arterial sistólica, pressão arterial diastólica e pressão arterial média. No pós-operatório avaliou-se a analgesia pela escala de Glasgow Modificada aos 30, 60, 120, 240 e 360 minutos. Não houve diferenças entre os parâmetros clínicos (p > 0,05) no período transoperatório entre e dentro dos grupos. O GEBI apresentou maior quantidade de resgates analgésicos transoperatórios (9) em relação a GALT (5), porém sem diferenças estatísticas. No pós-operatório, nenhum animal de ambos os grupos atingiu pontuação máxima para resgate analgésico. Pode-se concluir que a anestesia epidural associada ao bloqueio intercostal é uma técnica alternativa para casos em que se tenham limitações para utilização da anestesia local tumescente.
Palavras–chave: Tumores mamários; dor; anestesia locorregional; opioide.
Section: Medicina Veterinária
Received
June 18, 2018.
Accepted
March 19, 2020.
Published
JJune 16, 2020.
www.revistas.ufg.br/vet
visit the website to get the how to cite in the article page.
Introduction
Mammary tumors are the most common neoplasms in female dogs, and the recommended treatment in these cases is surgical resection. However, this type of surgery promotes extensive tissue divulsion, leading to moderate to severe pain(1). To avoid serious consequences caused by the acute postoperative pain, mastectomies should be performed under adequate analgesic and anesthetic techniques(2).
Trans- and postoperative pain is controlled through the use of a multimodal approach, which combines the use of drugs with different mechanism of action and non-pharmacological techniques(3). Opioids are widely used in acute pain control; however, studies in humans report that opioids cause negative impacts on the immune system, such as immunosuppression and inhibition of the action of natural killer cells(4), thereby questioning their use in cancer patients. In this context, recent studies suggest that local anesthetics can enable a significant decrease in the use of opioids and other immunosuppressive drugs, thus contributing to better prognosis.
Locoregional anesthesia is an element of multimodal pain management and is widely used in veterinary medicine because it reduces the operative use of general anesthetics and analgesics. Tumescent local anesthesia (TLA) is the most commonly used approach in dogs undergoing mastectomy and involves the administration of large amounts of diluted anesthetic solution in the subcutaneous tissue capable of promoting trans- and postoperative analgesia(5). However, there are limitations to its use, as in the case of poorly defined tumors, skin infection, or ulcerated tumors, owing to the risk of postoperative infection or seeding of neoplastic cells(6).
Epidural anesthesia promotes prolonged anesthesia as well as analgesia trans- and postoperation when associated with opioids with a shorter latency period(7); it is also used in surgeries of the pelvic limbs, tail, rectum, vagina, and abdomen(8,9). The ventral branches of the thoracic vertebrae in canines provide innervation to the subcutaneous tissue and mammary glands in the thoracic areas(10), enabling the use of regional intercostal block as a complementary method to block epidural anesthesia in mastectomy.
In view of the limitations of using tumescent local anesthesia, as well as fewer studies on the use of epidural anesthesia associated with intercostal block for mastectomy in bitches, studies and research comparing both techniques are necessary to develop a safe and efficient technique that can replace the use of TLA when it is not indicated.
Therefore, this study aimed to evaluate the use of tumescent local anesthesia or epidural anesthesia associated with intercostal block during the trans- and postoperative periods in bitches undergoing unilateral radical mastectomy.
Material and methods
This study was approved by the Animal Ethics and Experimentation Committee of the Federal University of Pelotas (protocol number 2058).
Fourteen bitches with mammary neoplasms undergoing unilateral radical mastectomy were used. There were no restrictions on age, race, or tumor type. The animals under study were evaluated for heart rate, respiratory rate, capillary filling time, mucosal staining, rectal temperature, chest radiographs, blood counts, and biochemical tests for kidney and liver assessment. Those bitches with changes recorded in general clinical examinations; lung metastasis; and ulcerated, contaminated, and/or adherent neoplasms were excluded from this study.
The dogs received a combination of acepromazine (0.03 mg/kg) and morphine intramuscularly (0.3 mg/kg) as pre-anesthetic medication. After 15 min, venous catheterization anesthetic induction with propofol (2 to 6 mg/kg) and anesthetic maintenance with isofluorane through a calibrated vaporizer were carried out. The percentage of anesthetic induction was determined by assessing the reflexes and parameters defined by Guedel.
After this stage, the dogs were randomly allocated into two groups, each containing seven animals (n = 7). One group contained those undergoing tumescent local anesthesia (GALT group) and the other group contained those undergoing epidural anesthesia associated with intercostal block (GEBI group).
The tumescent solution consisted of 460 mL of Ringer's lactate, 40 mL of 2% lidocaine, and 0.5 mL of epinephrine, reaching to a final concentration of 0.16%. Tumescent local anesthesia was induced with the dog in the supine position, through a Klein cannula, at a dose of 15 mL/kg.
Dogs in the GEBI group were placed in sternal decubitus, in the sphinx position, for aseptic puncture of the lumbosacral epidural space and administration of 2% lidocaine (5 mg/kg) and morphine (0.1 mg/kg). Ten minutes after the induction of epidural anesthesia, an intercostal block in the lateral decubitus was performed, at the 12th to the 6th intercostal space, using 2% lidocaine (2 mg/kg), not exceeding a total dose of 7 mg/kg.
An elliptical incision was made around the mammary chain with a surgical margin of approximately 1 cm, followed by divulsion of the subcutaneous tissue, clamping and ligation of blood vessels, and cranial and caudal superficial epigastric artery. Resection of the breast tissue and irrigation of the surgical wound with saline solution were performed, followed by reduction of subcutaneous tissue with simple isolated and continuous stitches and dermography with intradermal stitches. As this was a clinical study, the surgeon did not follow standard procedures.
Surgical procedures lasted around 130 min in the GEBI group and 55 minutes in the GALT group.
To assess intraoperative nociception, the Comen START8000D parametric monitor was used, and the following parameters were evaluated: heart rate, systolic blood pressure, diastolic blood pressure, and mean arterial pressure. These parameters were measured at baseline (MN), immediately after skin incision (IP), at divulsion of inguinal (DMI) and thoracic (DMT) mammaries, at caudal superficial epigastric artery clamping (PES), at the start of dead space reduction (REM), and at the start of dermography (DER). For noninvasive blood pressure measurements, occlusive cuffs with 40% brachial circumference were used, and they were positioned under the metacarpal artery. Respiratory rate was assessed by viewing the respiratory balloon.
Transoperative analgesic rescue was performed when the dog presented signs of nociception, such as a 30% increase in heart rate, respiratory rate, or blood pressure in relation to baseline, through the administration of fentanyl (µg/kg, Fentanest®) through intravenous administration. There were no restrictions on the number of redemptions that were carried out to normalize the parameters.
Thirty minutes after the end of anesthesia, the dog was submitted to the first postoperative pain assessment (T0), using the modified Glasgow pain scale [5]. Four additional evaluations were performed: the first two with an hour interval between each (T1, T2) and the last two with a two-hour interval between each (T4, T6), totaling to 6 hours. Evaluations were performed by an evaluator who was blinded to the treatment used.
After the end of the surgical procedure, all dogs received meloxicam (0.2 mg/kg/IV, Maxicam®). Analgesic rescue was performed with morphine (0.2 mg/kg, Dimorf®), intramuscularly when the evaluated dog had a pain scale score compatible with moderate or severe pain (Glasgow scale score > 6).
The dogs were discharged from the hospital after the end of the evaluation. For oral use, meloxicam analgesia (0.1 mg/kg/SID/3 days, Maxicam®), tramadol hydrochloride (5 mg/kg/TID/5 days, Cloridrato de Tramadol), and dipyrone sódium (25 mg/kg/SID/5 days) were prescribed in addition to antibiotic therapy with cephalexin (25 mg/kg/BID/7 days, Cefalexina®).
Nonparametric variables were assessed using the Mann-Whitney U test to determine the significant difference between groups, and the Friedman test, followed by the Dunn test, to determine the significant difference between moments in the same group. Parametric variables were assessed using the ANOVA RM test, followed by Dunnett's test for the significant difference between moments, and Student's t-test for the significant difference between groups. Analgesic rescues using fentanyl were evaluated using Kaplan-Meier and log-rank test analyses and Fisher's test. Differences were considered significant at p ≤ 0.05.
Results
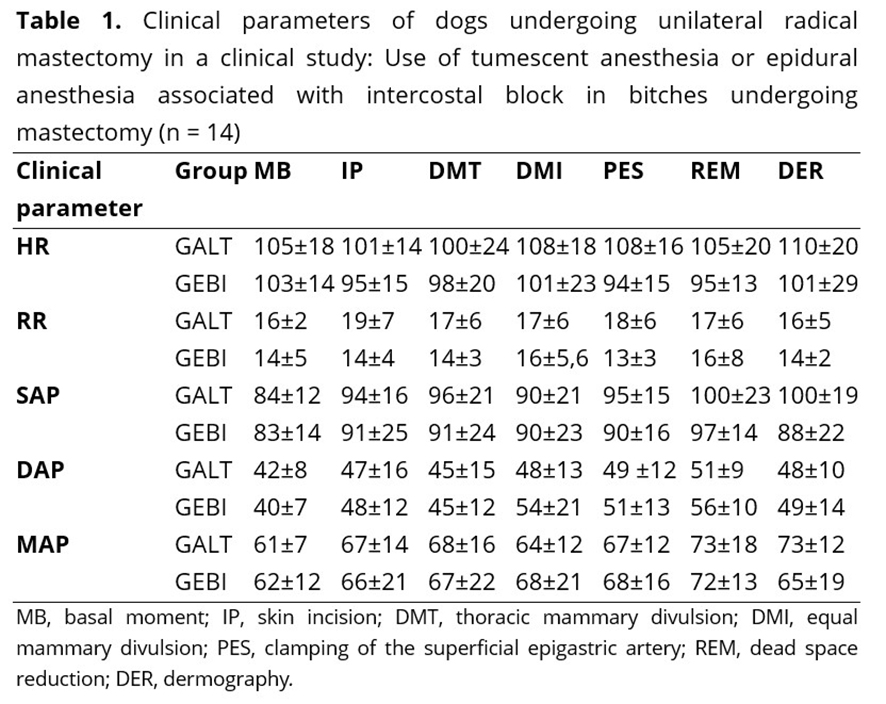
Regarding the clinical parameters evaluated in the transoperative period, there were no significant differences (p > 0.05) between moments in the same group compared to the baseline moment or between groups, as shown in Table 1.
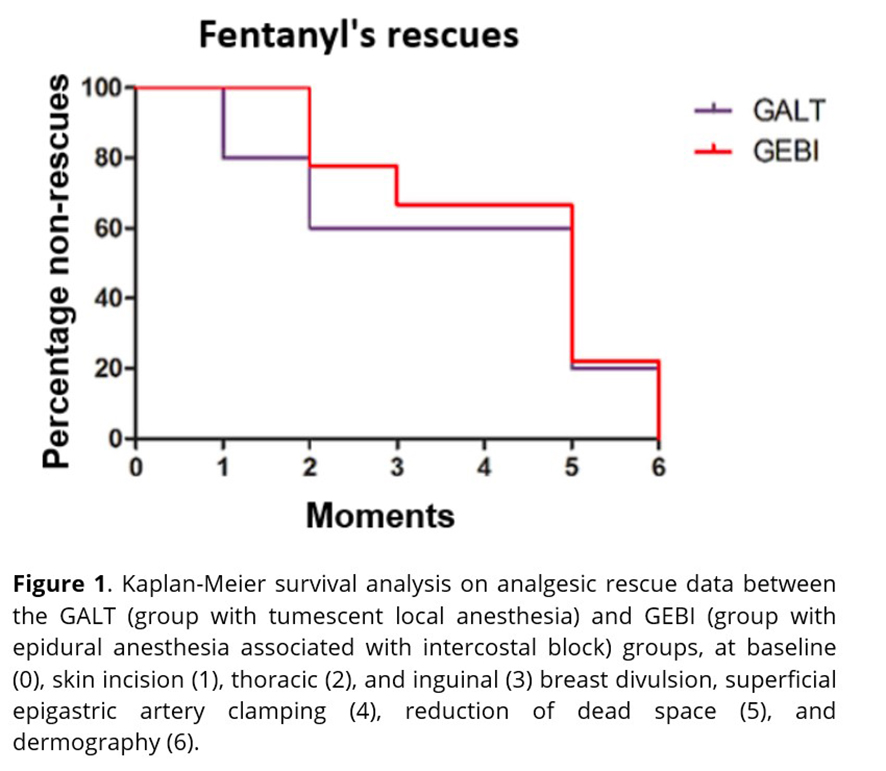
The GALT group showed 14.30% analgesic rescue at the time of IP, 14.30% in DMI, 0% in both DMT and PES, 28.30% in REM, and 14.30% in DER. The GEBI group showed 0% in IP, 28,30% in DMI, 14.30% DMT, 0% in PES, 57.20% in REM, and 28.30% in DER; however, there were no significant differences between the groups.
The dogs in the GEBI group showed a greater amount of analgesic rescue at the time of dead space reduction; however, there were no significant differences in surgical moments between the groups evaluated after performing Kaplan-Meier survival analysis, as observed in Figure 1.
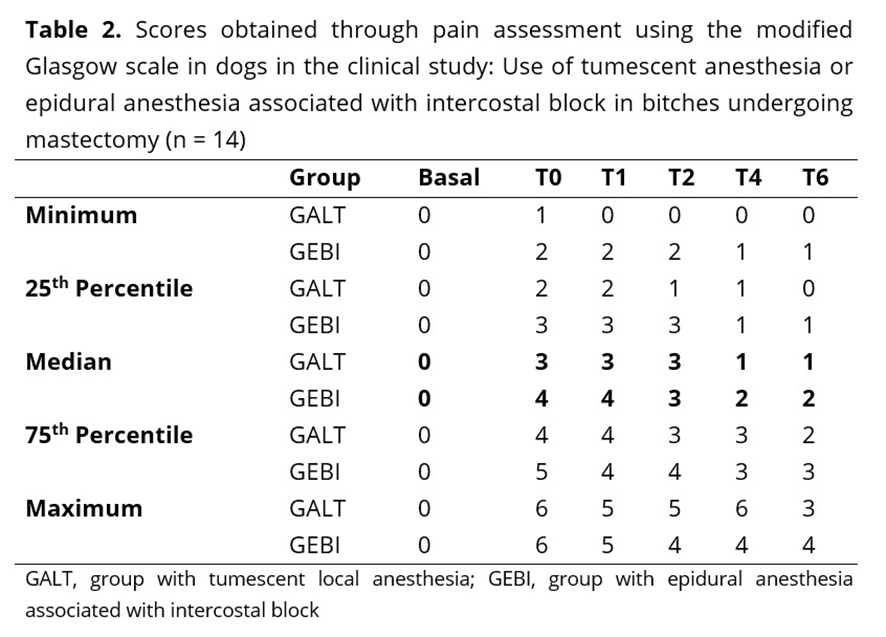
In both groups, the score compatible with moderate to severe pain was not reached, and there was no need for postoperative analgesic rescue. There were no significant differences between the groups, but within the same group, there was a significant difference between some moments and the baseline moment. In the GALT group, there was a significant difference between the baseline moment and the T0 and T1 times, and in the GEBI group, there was a significant difference between the baseline moment and T0 and T1 times (Table 2).
Discussion
There were no significant differences in systolic arterial pressure (SAP), mean arterial pressure (MAP), and diastolic arterial pressure (DAP) between the groups. However, two dogs in the GEBI group had SAP values below 90 mmHg in reducing dead space and divulsion of the thoracic breast, one of which was responsive to a reduction in the concentration of inspired isofluorane and an increase in the rate of fluid therapy, from 5 to 10 mL/kg of Ringer's lactate, and the other received vasoactive drugs (ephedrine, 0.1 mg/kg/IV).
Regarding heart rate, the results obtained in both groups did not show significant differences, corroborating what has already been mentioned by other authors who compared the use of tumescent local anesthesia in relation to the fentanyl bolus(5) and who evaluated the transoperative analgesia of epidural anesthesia associated with intercostal block(11). The results obtained in the respiratory rate assessment are in line with those obtained in a previous study, in which there were no significant differences between TLA and the use of continuous infusion of fentanyl(12).
In the present study, five dogs in the GEBI group and three dogs in the GALT group required analgesic rescue at some point during the surgical procedure, demonstrating that both locoregional techniques did not provide adequate transoperative analgesia at all times. We hypothesized that in the GALT group, rescue occurred because the tumescent solution concentration was lower than that previously described in the literature(12) or because of their poor distribution due to the body size of the dog(5). In the study conducted by Aguirre et al.(13), the concentration of the tumescent solution used was 0.16%, but they evaluated the data only during the postoperative period, not during the transsurgical period. This result is contrary to that reported in other studies, in which patients who underwent tumescent local anesthesia did not require a bolus of fentanyl at any time during surgery(5, 12).
In the GEBI group, analgesic rescue occurred largely when the dead space was reduced (57.20%). The present study is thus characterized as a clinical study, being carried out according to clinical routine without standardization by the surgeon. It is assumed that the prolonged time of the surgical procedure decreased the sensitive blockade of lidocaine, requiring analgesia supplementation. Other factors for future investigation include the possible migration of the catheter at the time of injection of the local anesthetic(14) and whether the dispersion of the local anesthetic in the epidural space does not occur uniformly because of the lateral decubitus position adopted to perform the intercostal block(15).
Regarding the evaluation of postoperative pain, the results obtained demonstrate that both techniques described in the different groups were effective for analgesia up to 6 hours after the surgical procedure, with no need for analgesic rescue. The GALT result is in line with what has already been described by Credie et al.(5) and Aguirre et al.(13), who found that TLA provides adequate postoperative analgesia; however, there are few reports on the use of epidural anesthesia associated with intercostal block for mastectomies in bitches. The results were similar to those obtained in the present study, indicating that the technique is effective for the postoperative period(11).
As the present study was considered a clinical study, we decided to use meloxicam in the immediate postoperative period due to the inflammatory issue of the surgical procedure and the need to mimic the clinical conditions used in the clinical routine. It is known that this administration may have a direct influence on postoperative analgesia because the analgesic efficacy of this drug has already been proven in mastectomies, in addition to reducing primary hyperalgesia in the surgical area by acting on the cyclooxygenase pathway, reducing the release of type E prostaglandins(16).
The significant differences perceived in the T0 and T1 times of the GALT group in relation to the postoperative pain assessment can be justified by the fact that the patients were still sedated, making the assessment difficult, a result similar to that found by other authors(13,17). In the GEBI group, the changes at moments T0, T1, and T2 are due to the same fact mentioned above because, in other studies, the sedative state was observed up to 2 h after the end of the anesthetic procedure(18) and the effect that the technique of epidural anesthesia has on the patient's ambulation in the first hours after surgery. Even with this limitation, the patients did not reach a score indicating analgesic rescue.
Conclusion
The use of epidural anesthesia associated with intercostal block and tumescent local anesthesia has a trans- and postoperative analgesic action of at least 6 hours and also possibly requires rescue in the trans-surgical period using both techniques in bitches subjected to unilateral mastectomy.
References